 Fioricet Side effects cannot be anticipated. If any develop or change in intensity, tell your doctor as soon as possible. Only your doctor can determine if it is safe for you to continue taking this drug. Fioricet Side effects may include: fatal skin reactions, seizure, confusion, depression, excitement, stomach pain, dizziness, drowsiness, intoxicated feeling, lightheadedness, nausea, sedation, shortness of breath, vomiting, excessive sweating.
Fioricet Side effects cannot be anticipated. If any develop or change in intensity, tell your doctor as soon as possible. Only your doctor can determine if it is safe for you to continue taking this drug. Fioricet Side effects may include: fatal skin reactions, seizure, confusion, depression, excitement, stomach pain, dizziness, drowsiness, intoxicated feeling, lightheadedness, nausea, sedation, shortness of breath, vomiting, excessive sweating.
Commonly reported side effects for Fioricet include:
- Euphoria
- Dizziness
- Drowsiness
- Intoxicated feeling
- Light-headedness
- Nausea
- Vomiting
- Sedation
- Substance dependence
- Shortness of breath
- Abdominal pain
Fioricet is implicated as causing repeat headaches with over-use.
Commonly reported side effects for Fioricet include:
- Euphoria
- Dizziness
- Drowsiness
- Intoxicated feeling
- Light-headedness
- Nausea
- Vomiting
- Sedation
- Substance dependence
- Shortness of breath
- Abdominal pain
Fioricet is implicated as causing repeat headaches with over-use
Fioricet Overdose
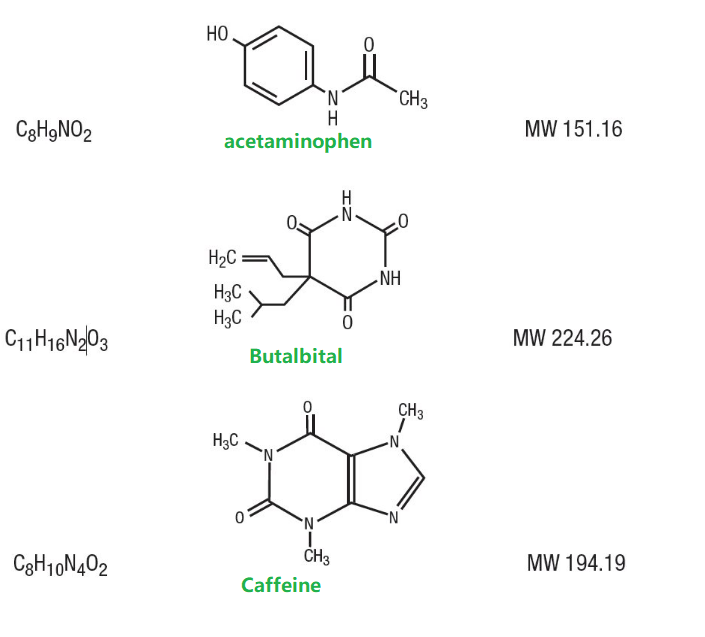
 The treatment of Fioricet overdose is complicated by the presence of two substances which are highly toxic when taken in excessive amounts. Fioricet overdoses generally result in toxic amounts of both acetaminophen and butalbital being consumed at once, requiring both overdoses to be treated at once. Fioricet overdose by anyone and/or any consumption by persons to whom it is not prescribed (particularly children) is always a medical emergency and medical attention must be sought immediately if an overdose or consumption by other persons is suspected.
The treatment of Fioricet overdose is complicated by the presence of two substances which are highly toxic when taken in excessive amounts. Fioricet overdoses generally result in toxic amounts of both acetaminophen and butalbital being consumed at once, requiring both overdoses to be treated at once. Fioricet overdose by anyone and/or any consumption by persons to whom it is not prescribed (particularly children) is always a medical emergency and medical attention must be sought immediately if an overdose or consumption by other persons is suspected.
Fioricet overdose is often fatal and symptoms may not present for hours following consumption; once initial overdose symptoms present they can progress rapidly and there may not be time to reach appropriate medical care after this point.
Acetaminophen exerts its toxicity through the production of a toxic metabolite which can sometimes produce liver damage with doses as low as 4,000 mg, although normally requiring doses that are much higher. Acute liver failure may result in doses greatly exceeding this, and death has been known to occur with ingestion of 10,000-15,000 mg (10-15 grams of pure acetaminophen).
The specific antidote to acetaminophen overdose is N-acetylcysteine. Acute renal failure and upper gastrointestinal bleeding may also occur.
Butalbital exerts its toxicity through excessive sedation resulting in respiratory depression and ultimately death via hypoxia. Nonlethal overdoses may also result in coma and death. There is no specific antidote to barbiturate overdose and treatment is supportive. Common treatment regimens generally include the administration of intravenous administration of saline, naloxone, thiamine, glucose, sodium bicarbonate to alkalize the urine to increase rate of excretion, and activated charcoal via nasogastric tube.
It is not uncommon for a doctor to recommend observation of the patient in the emergency department for a number of hours or admission to the hospital for several days of observation if symptoms are severe and to counsel the patient on drug abuse or refer them for psychiatric evaluation.

Fioricet Side Effects
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Lightheadedness
- shortness of breath
Incidence not known
- Abdominal or stomach pain
- black, tarry stools
- bleeding gums
- blistering, peeling, or loosening of the skin
- blood in the urine or stools
- blurred vision
- change in the frequency of urination or amount of urine
- chills
- cough
- diarrhea
- difficulty with breathing
- difficulty with swallowing
- dizziness
- drowsiness
- dry mouth
- fainting
- fast, pounding, or irregular heartbeat or pulse
- flushed or dry skin
- fruit-like breath odor
- hives, itching, or skin rash
- increased hunger
- increased thirst
- increased urination
- joint or muscle pain
- loss of appetite
- nausea or vomiting
- pinpoint red spots on the skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- red skin lesions, often with a purple center
- red, irritated eyes
- seizures
- shakiness in the legs, arms, hands, or feet
- sore throat
- sores, ulcers, or white spots in the mouth or on the lips
- sweating
- swelling of the feet or lower legs
- tightness in the chest
- trembling or shaking of the hands or feet
- troubled breathing
- unexplained weight loss
- unusual bleeding or bruising
- unusual tiredness or weakness
- weakness
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of overdose
- Confusion as to time, place, or person
- dark urine
- difficult or painful urination
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fever
- general feeling of discomfort or illness
- hallucinations
- headache
- holding false beliefs that cannot be changed by fact
- increased sweating
- irregular, fast or slow, or shallow breathing
- light-colored stools
- loss of appetite
- pale or blue lips, fingernails, or skin
- restlessness
- sudden decrease in the amount of urine
- sweating
- trouble sleeping
- unpleasant breath odor
- unusual excitement, nervousness, or restlessness
- vomiting of blood
- yellow eyes or skin
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Relaxed and calm
- sleepiness
Incidence not known
- Anxiety
- bloated
- constipation
- continuing ringing or buzzing or other unexplained noise in the ears
- depression
- earache
- excess air or gas in the stomach or intestines
- false or unusual sense of well-being
- full feeling
- hearing loss
- heartburn
- heavy eyelids
- high energy
- hot spells
- hyperventilation
- irritability
- numbness
- pain in the leg
- passing gas
- sluggishness
- stuffy nose
- tingling sensation
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.


 Avoid taking Fioricet with medications that affect your concentration, such as other narcotic pain relievers, general anesthetics, sleeping pills, anti-allergy medications, sedative-hypnotics, and tranquilizers (such as chlordiazepoxide). These may cause further drowsiness.
Avoid taking Fioricet with medications that affect your concentration, such as other narcotic pain relievers, general anesthetics, sleeping pills, anti-allergy medications, sedative-hypnotics, and tranquilizers (such as chlordiazepoxide). These may cause further drowsiness.


 Fioricet Side effects cannot be anticipated. If any develop or change in intensity, tell your doctor as soon as possible. Only your doctor can determine if it is safe for you to continue taking this drug. Fioricet Side effects may include: fatal skin reactions, seizure, confusion, depression, excitement, stomach pain, dizziness, drowsiness, intoxicated feeling, lightheadedness, nausea, sedation, shortness of breath, vomiting, excessive sweating.
Fioricet Side effects cannot be anticipated. If any develop or change in intensity, tell your doctor as soon as possible. Only your doctor can determine if it is safe for you to continue taking this drug. Fioricet Side effects may include: fatal skin reactions, seizure, confusion, depression, excitement, stomach pain, dizziness, drowsiness, intoxicated feeling, lightheadedness, nausea, sedation, shortness of breath, vomiting, excessive sweating. The treatment of Fioricet overdose is complicated by the presence of two substances which are highly toxic when taken in excessive amounts. Fioricet overdoses generally result in toxic amounts of both acetaminophen and butalbital being consumed at once, requiring both overdoses to be treated at once. Fioricet overdose by anyone and/or any consumption by persons to whom it is not prescribed (particularly children) is always a medical emergency and medical attention must be sought immediately if an overdose or consumption by other persons is suspected.
The treatment of Fioricet overdose is complicated by the presence of two substances which are highly toxic when taken in excessive amounts. Fioricet overdoses generally result in toxic amounts of both acetaminophen and butalbital being consumed at once, requiring both overdoses to be treated at once. Fioricet overdose by anyone and/or any consumption by persons to whom it is not prescribed (particularly children) is always a medical emergency and medical attention must be sought immediately if an overdose or consumption by other persons is suspected.

